Satya Medicherla1*, Guru Reddy2 and Shalabh Gupta3
1Preclinical Pharmacology, Unicycive Therapeutics, Inc., Los Altos, CA, United States
2Preclinical Research and Development, Unicycive Therapeutics, Inc., Los Altos, CA, United States
3Chairman of the Board of Directors and CEO, Unicycive Therapeutics, Inc., Los Altos, CA, United States
*Corresponding Author: Satya Medicherla, Preclinical Pharmacology, Unicycive Therapeutics, Inc., Los Altos, CA, United States.
Abstract
Background
There are no FDA approved drugs for the treatment of acute kidney injury (AKI). Inflammation- and reactive oxygen species-driven mitochondrial permeability transition pore (mPTP) opening causes mitochondrial dysfunction/swelling and cell death. This is implicated in acute diseases including AKI originating from ischemia-reperfusion (I/R) injury or delayed graft function. Additionally, unresolved inflammation exacerbates sustained mPTP opening and induces fibrotic lesions, evident in chronic kidney diseases. Nicotinamide adenine dinucleotide can suppress the frequency and duration of mPTP opening. UNI-494, a novel nicotinamide ester derivative and a selective mitochondrial ATP-sensitive potassium channel activator, reverses mitochondrial dysfunction by closing the mPTP. We present results from a study evaluating UNI-494’s efficacy in treating AKI in an I/R AKI rat model.
Methods
48 Sprague-Dawley rats were randomly assigned to 4 groups: one sham group and three I/R models. Rats were anesthetized, the right kidney was removed, and I/R was induced in the left kidney. I/R models received either no treatment or UNI-494 IV at 1 hour or 4 hours after ischemia. Blood and urinary samples were collected for AKI markers. The clamped left kidney was collected for tubular injury scores.
Results
UNI-494 at 10 mg/kg/IV reduced AKI markers and tubular injury scores in an AKI rat model compared to vehicle treated I/R group.
Conclusions
A single IV dose of UNI-494 at 10 mg/kg at 1 or 4 hours after ischemia significantly reduced the kidney functional markers and tubular injury scores. The data suggest UNI-494 slows down/reverses the progression of AKI in its established state.
Keywords
Acute Kidney Injury; UNI-494; Ischemia-Reperfusion; Acute Kidney Injury Treatment; Efficacy

Introduction
There are no FDA approved drugs for the treatment of acute kidney injury (AKI), which affects 10 – 15% of hospitalized patients and often results in renal transplantation or lifelong dialysis [1]. Mitochondrial dysfunction is a central factor in the development of AKI, as increased production of reactive oxygen species (ROS) by mitochondria contributes to cell death over time [2]. The mitochondrial permeability transition pore (mPTP) plays a critical role in mitochondrial dysfunction. First, increased ROS activates mPTP opening, which further increases ROS production [3,4]. Additionally, an inflammatory cascade elevates sustained mPTP opening in low-grade or chronic inflammation [3]. Thus, inflammation- and ROS-driven mPTP opening causes mitochondrial dysfunction/swelling [5,6]. This ruptures the outer mitochondrial membrane leading to subsequent apoptotic/necrotic cell death and is implicated in a wide range of acute diseases including AKI originating from ischemia-reperfusion (I/R) injury or delayed graft function (DGF) [7]. Next, the unresolved inflammation enhances sustained opening of mPTP [8], which eventually induces fibrotic lesions [9]. This is evident in a broad range of chronic diseases such as chronic kidney disease (CKD) originating from hypertension or hyperglycemia and/or inflammation driven fibrosis [10].
UNI-494 is a novel nicotinamide ester derivative that is a selective mitochondrial ATP-sensitive potassium channel (KATP) activator, which reverses the mitochondrial dysfunction by closing the mPTP. We present results from a study comparing rats with unilateral renal I/R treated with vs without intravenous (IV) UNI-494 to evaluate UNI-494’s efficacy in treating AKI. Unilateral renal I/R rat model of AKI is a well-established model of DGF [11].
Methods
Experimental animals
Jugular vein cannulated Sprague Dawley rats were purchased from Charles River Laboratories (Hollister, CA) to have body weights of approximately 250 – 275g at the start of the study. Following arrival, animals were singly housed in cages with micro-filtered tops using SaniChip bedding 7990A (Harlan Teklad, Hayward, CA), except as noted below for metabolic caging. Animal room controls were set to maintain temperature and relative humidity at 20°C ± 1°C and 50% ± 20%, respectively, with at least 10 air changes/hour. Housing rooms were on a 12-h:12-h light/dark cycle. Animals were provided with ad libitum access to water (via water bottles) and to a standard chow (2018 Teklad Global 18% Protein Rodent Diet; Harlan Teklad). Animals were acclimated on site for at least 7 days before initiation of the study.
Study design
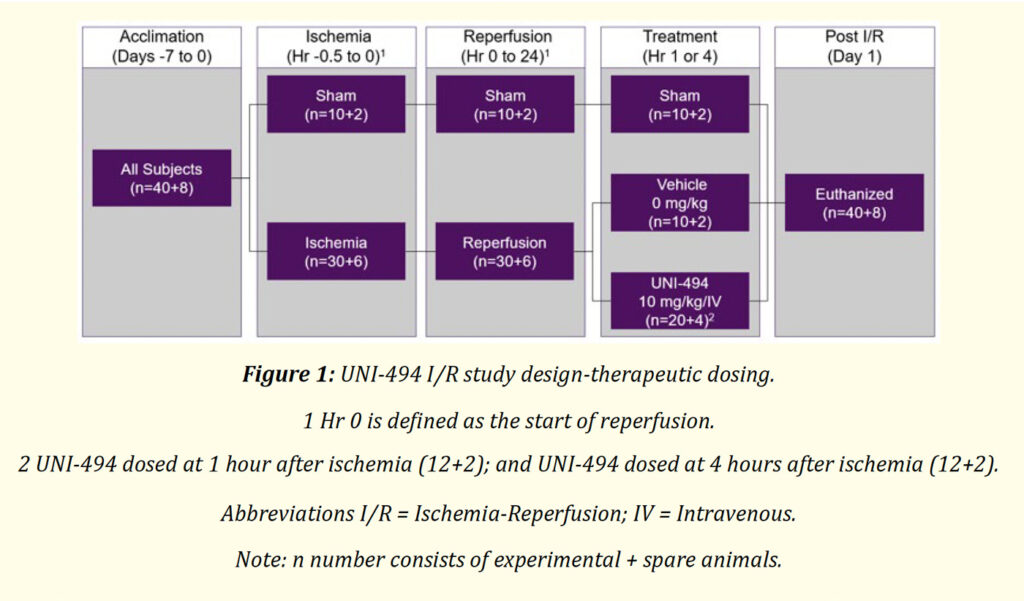
48 jugular vein cannulated Sprague-Dawley rats were randomly assigned to 4 groups (n = 10+2). One group was the Sham group and the other three groups were established as the I/R models. I/R models received either no treatment (vehicle), 10 mg/kg UNI-494 IV at 1 hour after ischemia, or 10 mg/kg UNI-494 IV at 4 hours after ischemia (Figure 1). The vehicle for IV formulation consisted of Sterile Water for Injection (WFI), which was obtained by the Testing Facility from a commercial vendor.
Figure 1: UNI-494 I/R study design-therapeutic dosing
Study procedures
Rats were anesthetized and the abdomen was opened at the midline. The right kidney was removed (right nephrectomy). Ischemic injury was induced in the left kidney by placing a small clip (Sugita standard aneurysm clip, holding force 145g; Mizuho Ikakogyo, Tokyo, Japan) on the renal vascular pedicle for 30 minutes. Removal of the clip was defined as the start of reperfusion (“0 hours”). Sham operations were performed in a similar manner, except that the right kidney was not removed, and the renal vessels were not clamped. At 0 hours (or the equivalent for sham-operated animals), each rat was moved to an individual metabolic cage for the collection of urine. UNI-494 was administered at 1 or 4 hours after ischemia with established renal injury confirmed by elevated serum creatinine (sCr).
Study assessments
After 24h of reperfusion, animals were anesthetized, subjected to terminal cardiocentesis, and euthanized without recovery. Collections were performed and processed as follows.
A volume of blood sufficient to provide 5 mL of serum was collected into serum separator tubes. Following centrifugation, the resulting serum from each animal was aliquoted to individual tubes (5 x 1 mL). The tubes then were flash-frozen on dry ice and stored at -20°C pending analysis. Subsequently, serum levels of Cr, neutrophil gelatinase-associated lipocalin (sNGAL), and blood urea nitrogen (sBUN) were determined in the non-acetic acid-stabilized samples using instruments/kits according to the respective manufacturer’s instructions.
The volumes and pH levels of the 24-h urine samples were recorded. The urine samples were aliquoted to individual tubes, flashfrozen on dry ice, and stored at -20°C pending analysis. Subsequently, urine levels of creatinine (uCr), albumin (uALB), and NGAL (uNGAL) were determined using kits according to the respective manufacturer’s instructions. The uCr and uALB values were used to calculate the uALB:uCre ratio (uACR).
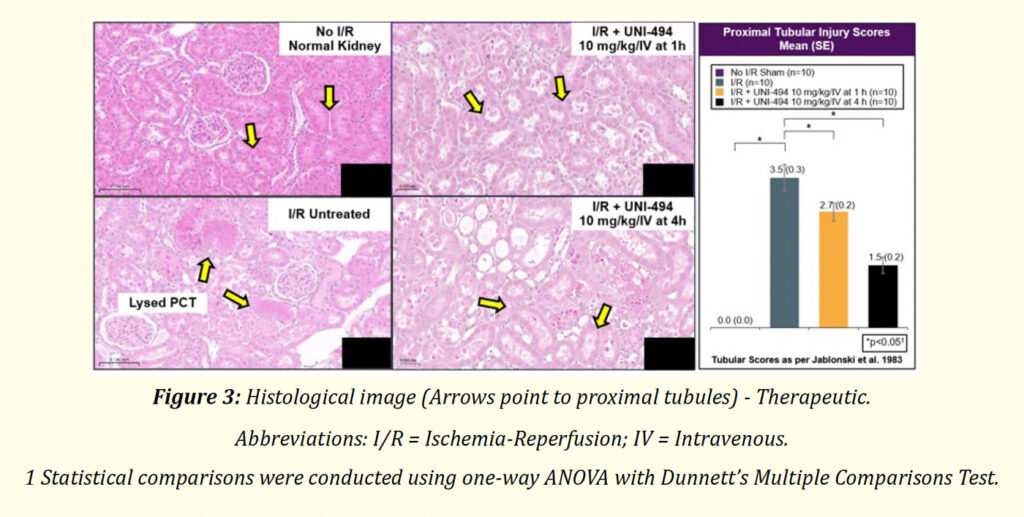
At necropsy, the left kidney of each animal was collected and fixed overnight in 10% neutral buffered formalin at room temperature, then stored in 70% ethanol at room temperature. Fixed tissues were processed, sectioned, and stained with hematoxylin and eosin. The resulting slides were transferred to the Sponsor-designated facility for histopathological evaluation, including scoring of tubular damage (necrosis, dilation, and casts), scoring of inflammation, and inspection for other renal changes (especially mitochondrial changes). Tissues were assessed for tubular injury using Jablonski., et al. (1983) proximal convoluted tubule scoring method (0 = No change present; 1 = Minimal; 2 = Mild; 3 = Moderate; 4 = Marked) [12]. Representative images of histopathological changes were derived from images captured with 3DHistech Pannoramic digital scanner.
Statistical analysis
Data were analyzed with a one-way ANOVA followed by Dunnett’s multiple comparison tests. A threshold of p < 0.05 was used to determine a significant difference between groups. Statistical Package for the Social Sciences (SPSS) was used for all statistical analyses.
Results
Kidney function analyses
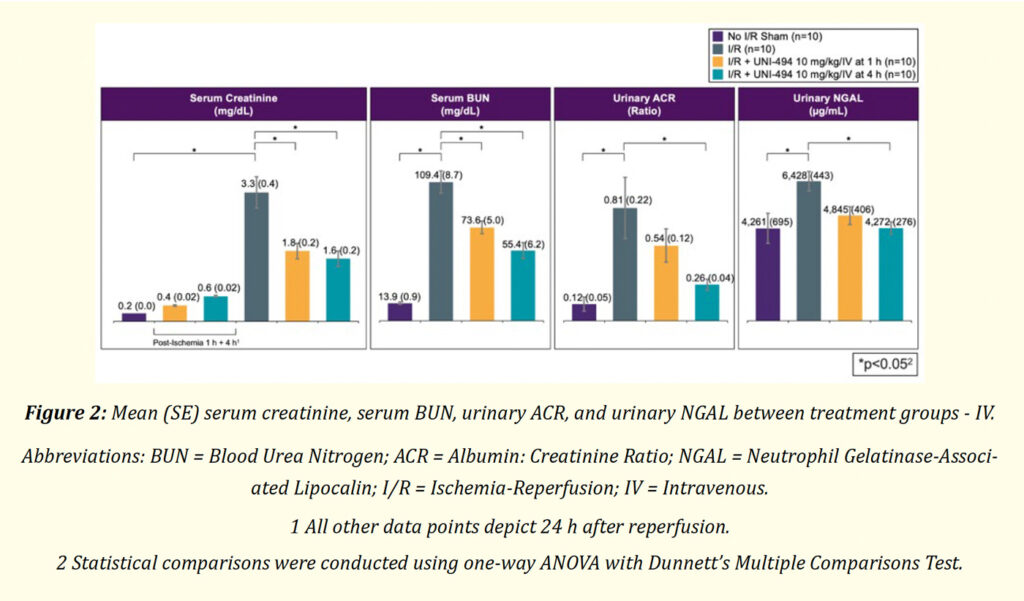
Renal injury was established by confirming elevation of sCr by 1 hour and 4 hours after ischemia in the UNI-494 groups (Figure 2). At 24 hours, I/R induced significant increases of sCr, sBUN, uACR, uNGAL, and tubular injury scores in the vehicle treated I/R group compared to the no I/R sham group (p < 0.05, ANOVA with Dunnett’s Multiple Comparisons Test) (Figure 2 and 3). A 10 mg/kg/IV UNI-494 dose consistently reduced AKI markers compared to the vehicle treated I/R group (p < 0.05 for sCR and sBUN at 1 and 4 hours, p <0.05 for uACR and uNGAL at 4 hours) (Figure 2). Mean sCr for I/R groups administered UNI-494 at 1 and 4 hours were 1.8 and 1.6 mg/dL, respectively, compared to 3.3 mg/dL in the vehicle treated I/R group (Figure 2). Mean sBUN for I/R groups administered UNI-494 at 1 and 4 hours were 73.6 and 55.4 mg/dL, respectively, compared to 109.4 mg/dL in the vehicle treated I/R group. Mean sNGAL for I/R groups administered UNI-494 at 1 and 4 hours were 2140 and 1587 μg/dL, respectively, compared to 4961 μg/dL in the vehicle treated I/R group. Mean uALB for I/R groups administered UNI-494 at 1 and 4 hours were 148 and 81 μg/mL, respectively, compared to 283 μg/mL in the vehicle treated I/R group. Mean uACR for I/R groups administered UNI-494 at 1 and 4 hours were 0.54 and 0.26 mg/dL, respectively, compared to 0.81 mg/dL in the vehicle treated I/R group (Figure 2). Mean uNGAL for I/R groups administered UNI-494 at 1 and 4 hours were 4845 and 4272 μg/mL, respectively, compared to 6428 μg/mL in the vehicle treated I/R group (Figure 2).
Figure 2: Mean (SE) serum creatinine, serum BUN, urinary ACR, and urinary NGAL between treatment groups – IV.
A 10 mg/kg/IV UNI-494 dose also reduced proximal tubular necrosis/injury and decreased tubular injury scores compared to the vehicle treated I/R group (p < 0.05, ANOVA with Dunnett’s Multiple Comparison Test) (Figure 3).
Figure 3: Histological image (Arrows point to proximal tubules) – Therapeutic
Safety
There were no mortalities during any phase of the study. All the rats in the study survived to the scheduled euthanasia time point. No clinical observations were noted during any phase of the study.

DISCUSSION
There are no FDA approved drugs for the treatment of AKI, which affects 10 – 15% of hospitalized patients and often results in renal transplantation or lifelong dialysis [1]. Mitochondrial dysfunction is implicated in the pathology of various acute diseases, including AKI [7] and the mPTP is crucial to mitochondrial dysfunction. Over time, inflammation- and ROS-driven mPTP opening leads to mitochondrial dysfunction and swelling [5,6]. This ruptures the outer mitochondrial membrane, subsequently triggering apoptotic/necrotic cell death, and is associated with various acute diseases, including AKI originating from I/R injury or DGF [7]. Additionally, persistent inflammation worsens ongoing mPTP opening [8], which is evident in CKD [10]. Nicotinamide adenine dinucleotide can suppress the frequency and duration of mPTP opening. UNI-494 is a novel nicotinamide ester derivative that is a selective mitochondrial KATP activator, which is expected to reverse the mitochondrial dysfunction by closing the mPTP.
The objective of the study was to evaluate the in vivo efficacy of IV UNI-494 in the unilateral renal I/R rat model of AKI, which is a well established model of DGF [11]. To our knowledge, this is the first preclinical study to evaluate the efficacy of IV UNI-494 in the unilateral renal I/R rat model of AKI.
Study results clearly demonstrated that induction of I/R increased AKI markers and injured proximal tubules, and that one dose of UNI-494 at 10 mg/kg/IV administered after ischemia induction effectively reduced AKI markers and proximal tubule injury scores in an AKI rat model. I/R of the kidney caused both glomerular dysfunction (as represented by the biomarkers sCr, sBUN and uACR) and tubular dysfunction (as represented by the biomarker uNGAL and proximal tubular injury scores). Notably, therapeutic administration of UNI-494 decreased both glomerular and tubular dysfunction. These data stand in contrast to previously published models of nicorandil, which provided greater beneficial action against tubular dysfunction compared to glomerular dysfunction [13]. Overall, our study results suggest that therapeutic administration of UNI-494 slows the progression of, halts, or even reverses AKI.
The main limitation is that our study evaluated UNI-494 efficacy in a rat model. Future studies should evaluate UNI-494 efficacy in humans.
UNI-494 is a potential candidate for the treatment of DGF and other AKI clinical conditions. The mechanism of this potential therapeutic effect should be further investigated. Studies evaluating this promising treatment in the target population of patients with AKI should be conducted.
CONCLUSIONS
UNI-494 is a novel nicotinamide ester derivative that is a selective mitochondrial KATP activator, which reverses mitochondrial dysfunction by closing the mPTP. A single IV dose of UNI-494 at 10 mg/kg at 1 or 4 hours after ischemia significantly reduced the kidney functional markers sCr, sBUN, uACR, uNGAL, and tubular injury scores. These data indicate that therapeutic administration of UNI-494 potentially stops or even reverses the progression of AKI.
Acknowledgements
Editorial support was provided by Xelay Acumen Group, Inc. (funded by Unicycive Therapeutics, Inc.). All the authors have authorized the submission of their manuscript via Xelay Acumen Group, Inc. and have approved all statements and declarations, including conflicting interests and funding.
Ethics Approval
The procedures that were applied to animals in this protocol were approved by the MuriGenics Inc. Institutional Animal Care and Use Committee. The care and use of animals were conducted in accordance with the regulations of the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC).
Informed Consent to Participate
Informed consent was not necessary because this was a preclinical study in rats.
Competing Interests
Satya Medicherla, Guru Reddy, and Shalabh Gupta are employees of Unicycive Therapeutics, Inc.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. Restrictions apply to the availability of data generated or analyzed during this study because they were used under license. The corresponding author [satya.medicherla@unicycive.com] will on request detail the restrictions and any conditions under which access to some data may be provided.
Funding Acknowledgement
The study was funded by Unicycive Therapeutics, Inc.
Bibliography:
- Goyal A., et al. “Acute Kidney Injury”. Statpearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC., (2024).
- De Giorgi F., et al. “The permeability transition pore signals apoptosis by directing Bax translocation and multimerization”. FASEB Journal 16.6 (2002): 607-609.
- Kent AC., et al. “Targeting the mitochondrial permeability transition pore to prevent age-associated cell damage and neurodegeneration”. Oxidative Medicine and Cellular Longevity (2021): 6626484.
- Zorov DB., et al. “Reactive oxygen species (Ros)-Induced Ros release: A new phenomenon accompanying induction of the mitochondrial permeability transition in cardiac myocytes”. Journal of Experimental Medicine 192.7 (2000): 1001-1014.
- Kinnally KW., et al. “Is Mptp the gatekeeper for necrosis, apoptosis, or both?” Biochimica et Biophysica Acta 1813.4 (2011): 616-622.
- Hunter DR and RA Haworth. “The Ca2+-induced membrane transition in mitochondria. I. The protective mechanisms”. Archives of Biochemistry and Biophysics 195.2 (1979): 453-459.
- Zhang X., et al. “The role of mitochondria in acute kidney injury and chronic kidney disease and its therapeutic potential”. International Journal of Molecular Sciences 22.20 (2021): 11253.
- Endlicher R., et al. “The mitochondrial permeability transition pore-current knowledge of its structure, function, and regulation, and optimized methods for evaluating its functional state”. Cells 12.9 (2023): 1273.
- Zhang S., et al. “Postconditioning protects renal fibrosis by attenuating oxidative stress-induced mitochondrial injury”. Nephrology Dialysis Transplantation 32.10 (2017): 1628-1636.
- Irazabal MV and VE Torres. “Reactive oxygen species and redox signaling in chronic kidney disease”. Cells 9.6 (2020): 1342.
- Cavaillé-Coll M., et al. “Summary of FDA workshop on ischemia reperfusion injury in kidney transplantation”. American Journal of Transplantation 13.5 (2013): 1134-1148.
- Jablonski P., et al. “An experimental model for assessment of renal recovery from warm ischemia”. Transplantation 35.3 (1983): 198-204.
- Shimizu S., et al. “Nicorandil ameliorates ischaemia-reperfusion injury in the rat kidney”. British Journal of Pharmacology 163.2 (2011): 272-282.